Overview
The Hospice Timing panel includes two tables that provide a detailed analysis that demonstrates the impact of earlier and longer hospice care. The content in this panel proves that earlier and longer hospice care for the selected provider's patients correlates with lower overall Medicare spend and reduced healthcare utilization in a patient’s final months of life.
There are two related tables in the gray panel.
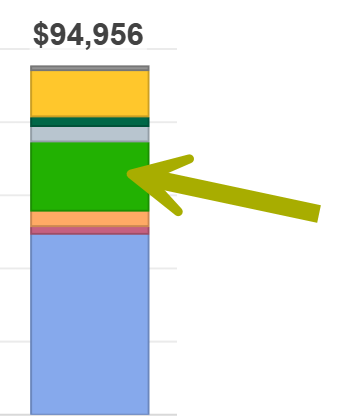
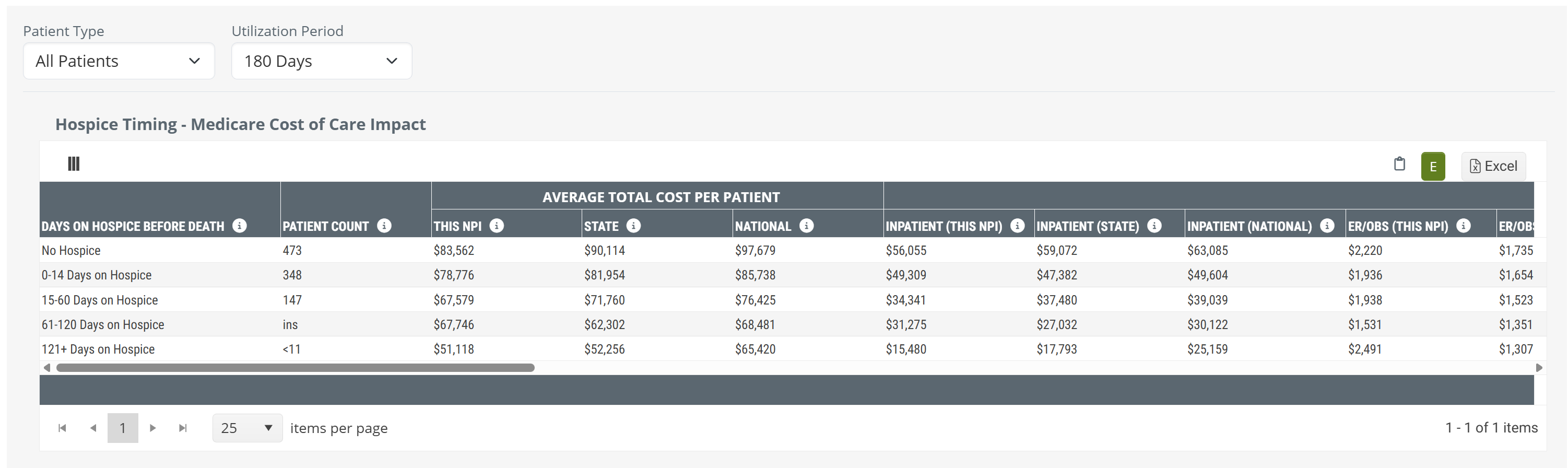
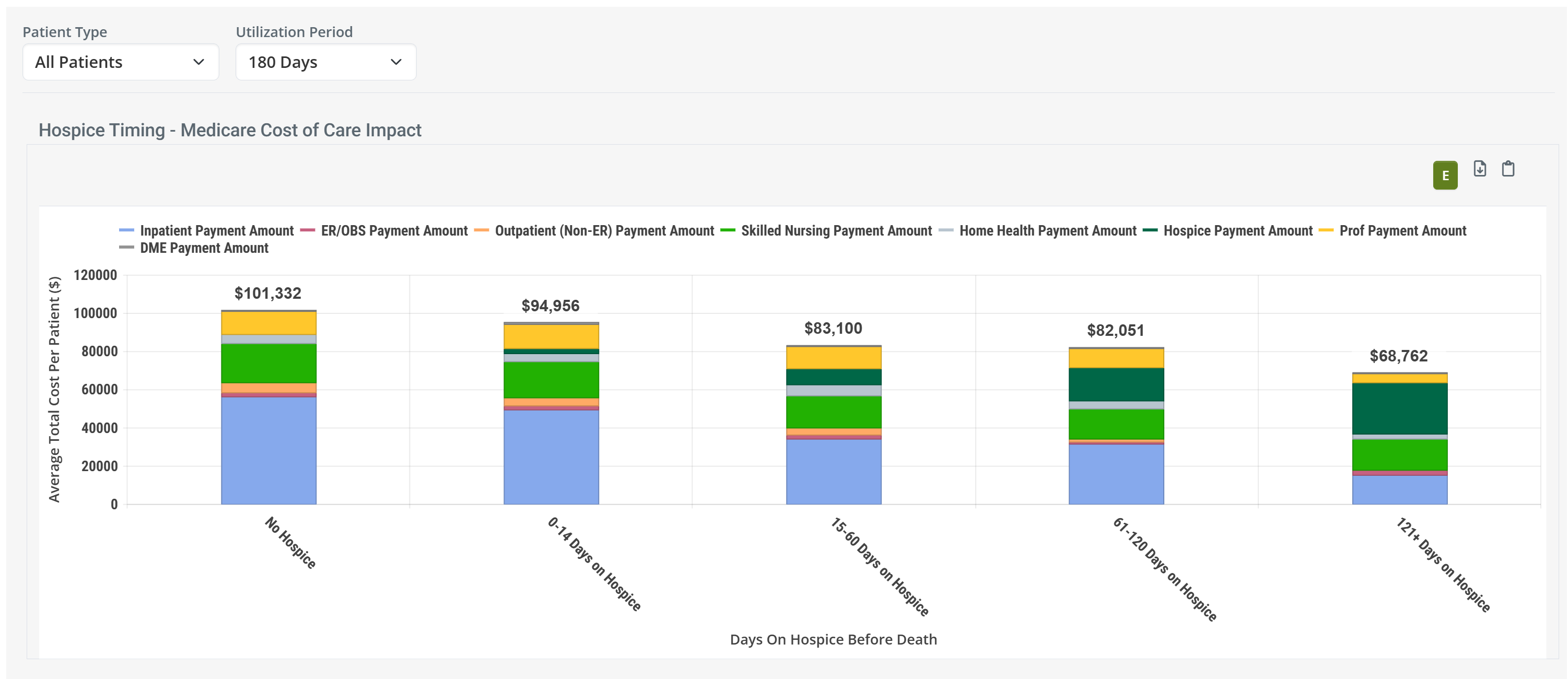
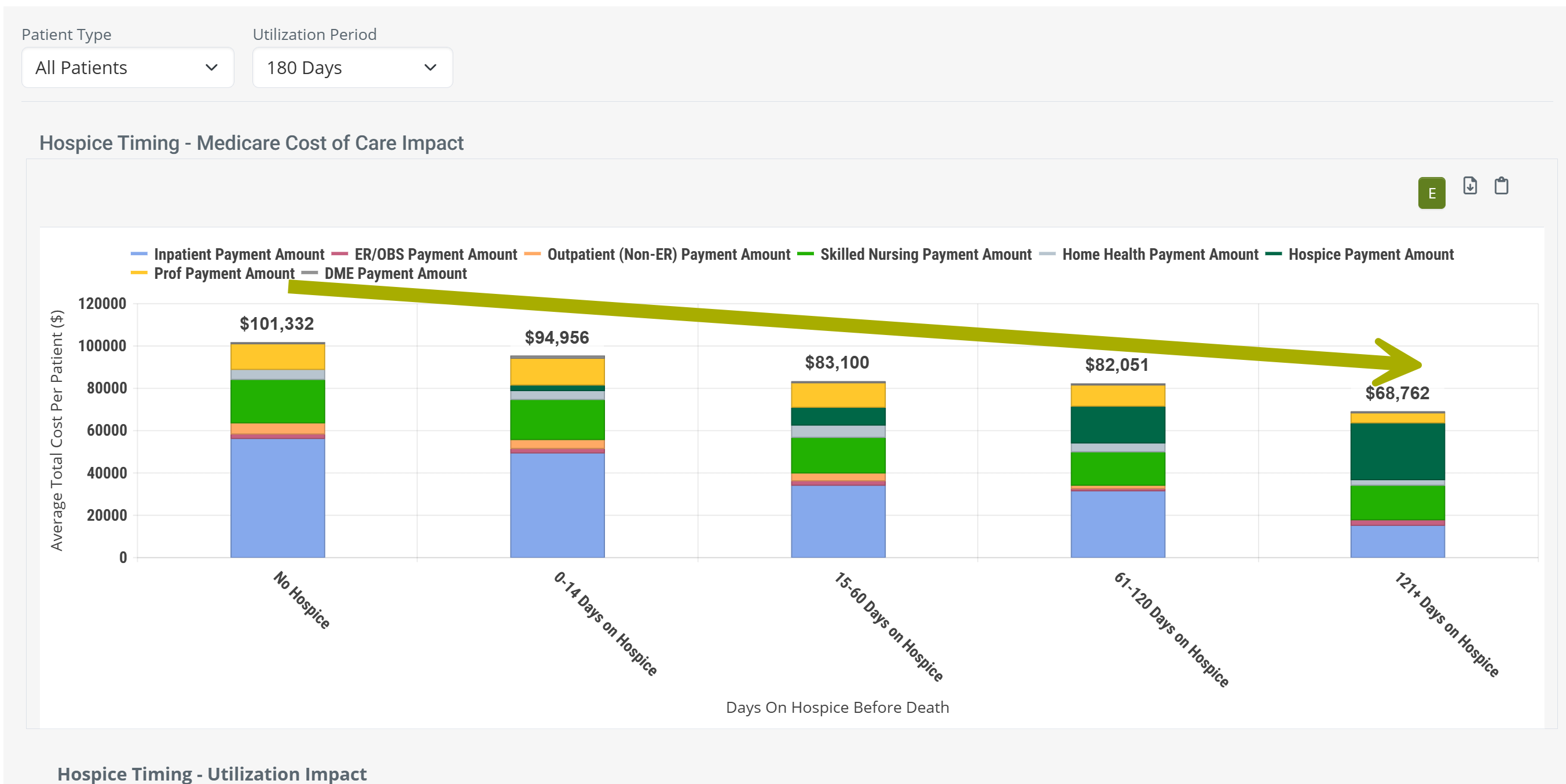
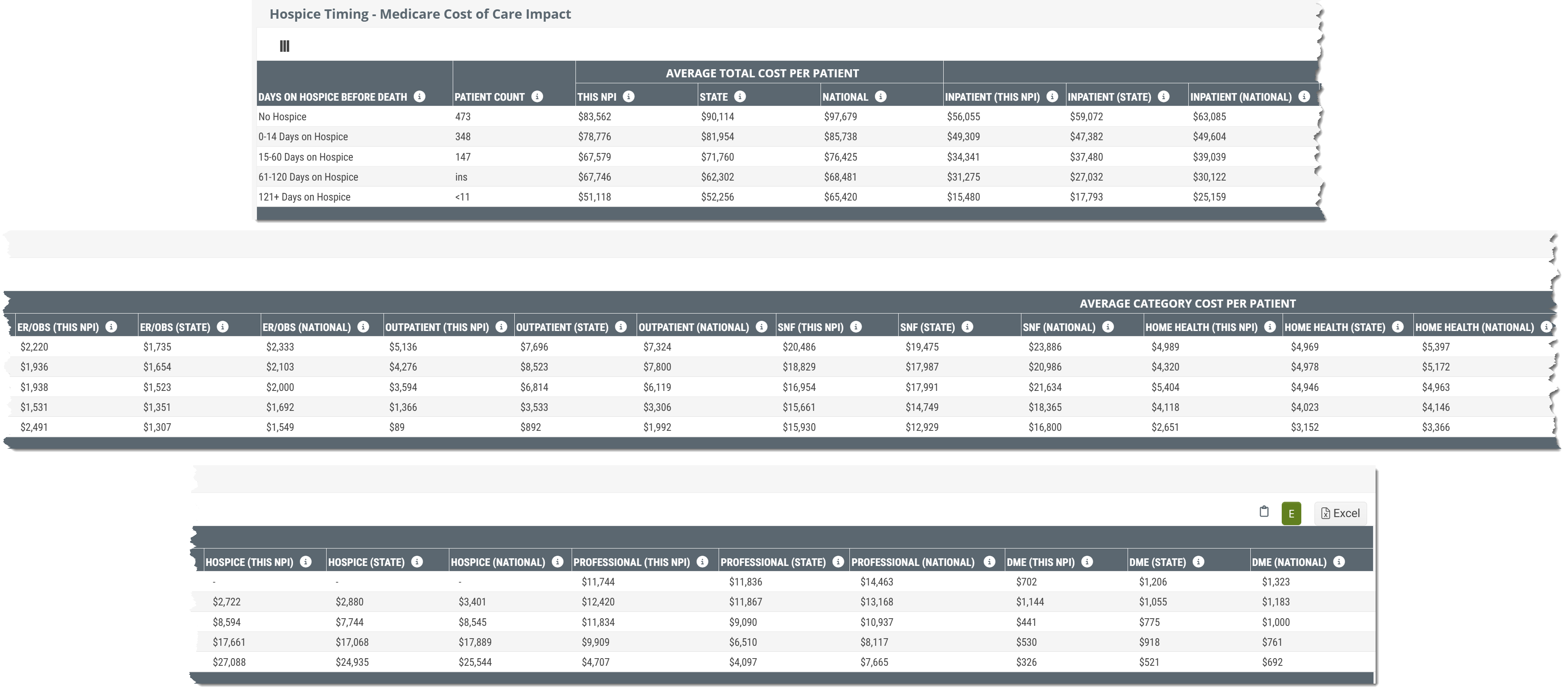
- Hospice Timing - Medicare Cost of Care Impact - shows costs of care for hospice patients during different periods of time, and for different patient types. This can be displayed as a chart or a table.
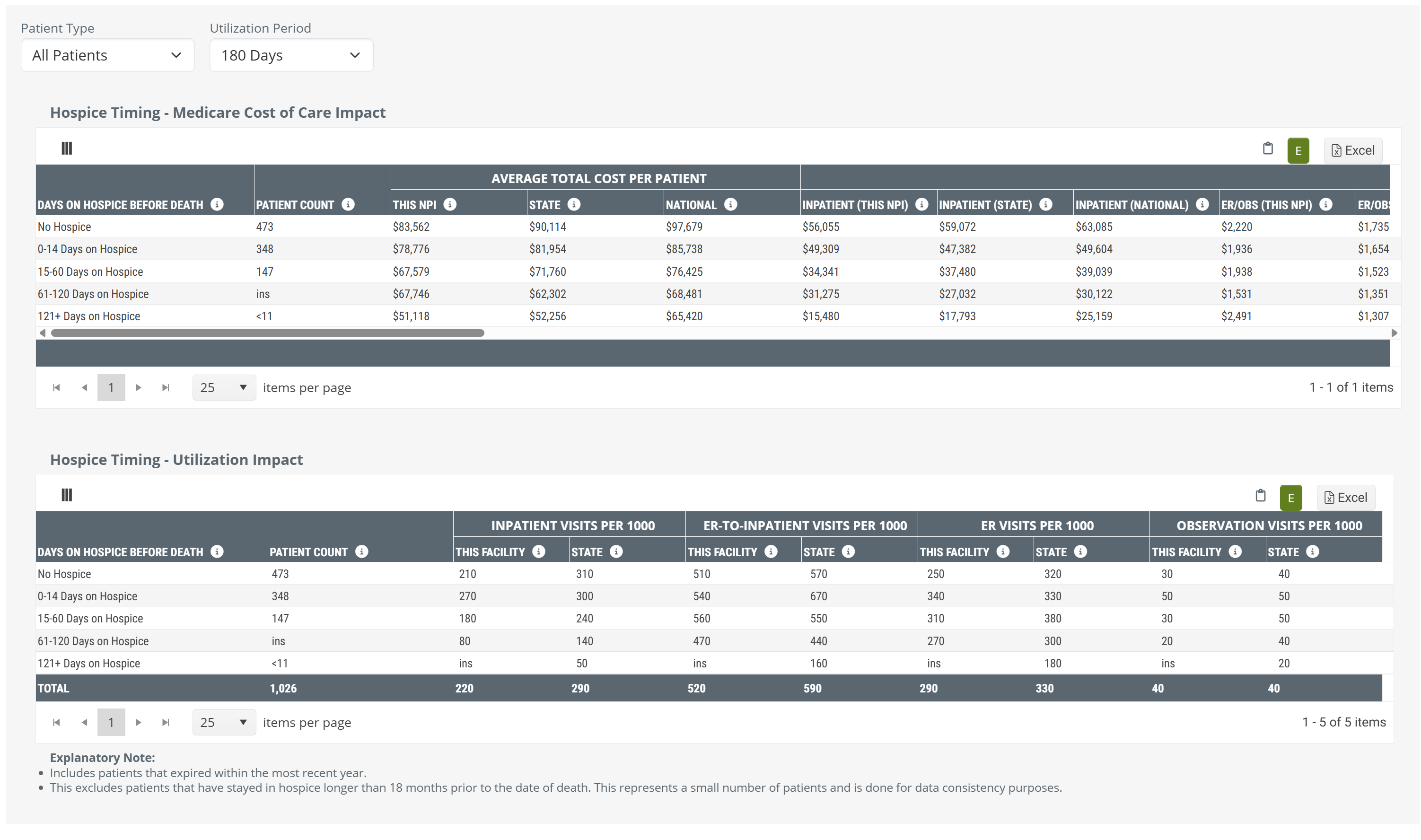
- Hospice Timing - Utilization Impact - focuses specifically on the impact of patient utilization. You can see how earlier hospice care impacts subsequent ER, OBS, and inpatient admissions.
 Physicians and Facilities
Physicians and Facilities
The Hospice Timing panel is available on the Facility Analyze page, under the Utilization & Quality tab and on the Physician Analyze page under the Utilization tab. The metrics displayed reflect the selected provider; physician or hospital, but the structure of the panel and the metrics displayed in the tables, or chart, are essentially identical, and the features work the same.
![]() For the few differences, see The difference between Physicians Analyze and Hospitals Analyze
For the few differences, see The difference between Physicians Analyze and Hospitals Analyze
 In this article
In this article
- Value Summary - a list of the available insights from the Hospice Timing panel
- The difference between Physicians Analyze and Hospitals Analyze
-
Panel Settings
- Chart View - you can view the Medicare Cost of Care content as a table or a chart
- Filters - you can select a very specific patient population to evaluate
- Hospice Timing - Medicare Cost of Care Impact table or chart
- Hospice Timing - Utilization Impact table
- Why do we use "Visits per 1000"
 Value
Value
Value Summary - It is impossible to overstate how conclusively these detailed hospice timing metrics prove that getting patients into hospice care earlier positively impacts costs and utilization. Consider the following:
 Quantifies impact with real patient data
Quantifies impact with real patient data
The tables provide proof that you can provide to referring physicians and facilities how the timing of hospice enrollment affects their own patients spend, utilization, and care intensity.
 Reveals high value education opportunities
Reveals high value education opportunities
The tables demonstrate the impact of late transitions and how they result in unnecessary hospitalizations, readmissions, or higher spend — arming reps with objective, claims-backed talking points.
 Provides state and national benchmarks for comparison
Provides state and national benchmarks for comparison
The metrics in these tables contextualize performance against broader trends, helping organizations uncover gaps and opportunities for improvement.
 Supports value-based care alignment
Supports value-based care alignment
The tables enable providers to demonstrate the financial and clinical benefits of timely hospice enrollment to partners seeking improved quality and coordination.
![]() The point of all of the metrics in these tables is to prove the value of earlier hospice for dying patients. To do so, all of the costs during the time periods are calculated backward from the deaths of the patients included in the metrics.
The point of all of the metrics in these tables is to prove the value of earlier hospice for dying patients. To do so, all of the costs during the time periods are calculated backward from the deaths of the patients included in the metrics.
The difference between Physicians Analyze and Hospitals Analyze
The Hospice Timing panel is available for both hospitals and physicians. The metrics displayed in the panel are the same for physicians and hospitals, and so is the value of the insights the tables in the panel provide
However, there are a few differences which are shown in the table below.
Physicians |
Hospitals |
|
| Where found | Physician Analyze page under the Utilization tab. | Facility Analyze page under the Utilization and Quality tab. |
| Count details | The metrics in the table, for physicians, are based on counts of patients who died during the one-year reporting period and were treated by the physician within six months prior to the death date | The metrics in the table, for hospitals, are based on counts of patients deceased during the most recent 4 quarters, who were admitted to the selected facility up to 6 months prior to death. |
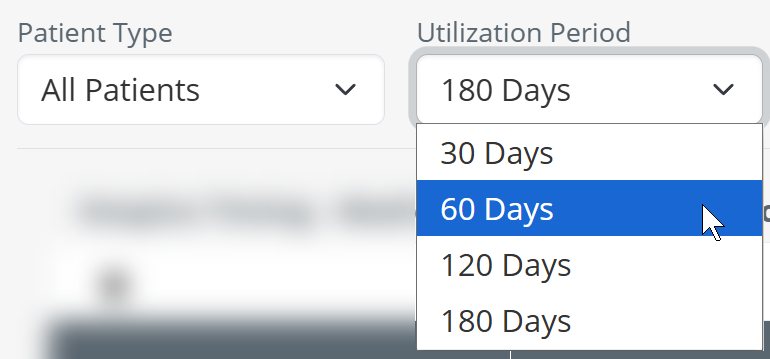
| Utilization filter | For the Utilization filter on the Physician Analyze page, you can select a period of 30, 60, or 180 days. | For the Utilization filter on the Facility Analyze page, you can select a period of 30, 60, 120, or 180 days. |
Panel Settings
There are some basic settings for the Hospice Timing panel that allow you to customize what content is displayed in the panel and how it is displayed. This includes Chart View and Filters.
Chart View
At the top left of the page you will find a toggle icon that allows you to turn chart view on and off. With chart view on, the chart is shown for the Hospice Timing - Medicare Cost of Care Impact table.
The following images show the difference between chart view off and chart view on for the Hospice Timing panel.
Filters
This panel provides flexibility that allows you to evaluate hospice timing for different patient populations for the selected provider. Each dropdown selector is described below.
![]() The specific metrics that appear in both tables are determined by the choices you make.
The specific metrics that appear in both tables are determined by the choices you make.
|
Patient Types - this dropdown allows you to choose between three patient type categories. Each are described below.
|
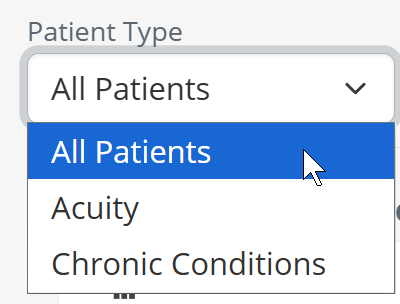 |
| All Patients - with this selection, all patients discharged from the selected provider will be used to calculate the metrics shown in the table. | 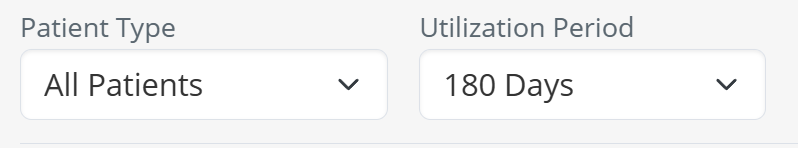 |
|
Utilization Period - You can select the length of time from which patients will be included in the calculations for the metrics in the table.
|
 |
|
Acuity - You can select to filter patients by their acuity.
|
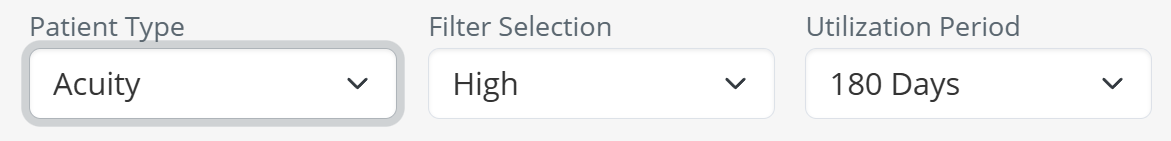 |
| Acuity Level - if you use the Acuity patient type, you can then use the second dropdown to choose a specific acuity level. | 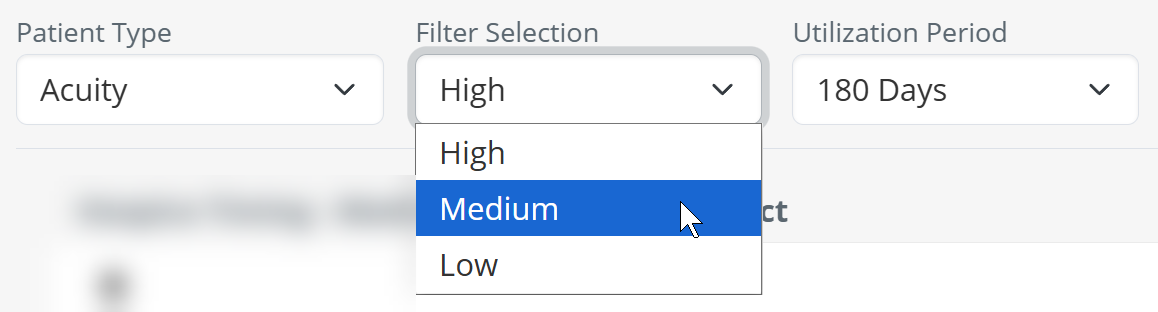 |
| Utilization Period - once you have chosen an acuity level, you can choose to filter the results in the table to a specific period using the third dropdown. | 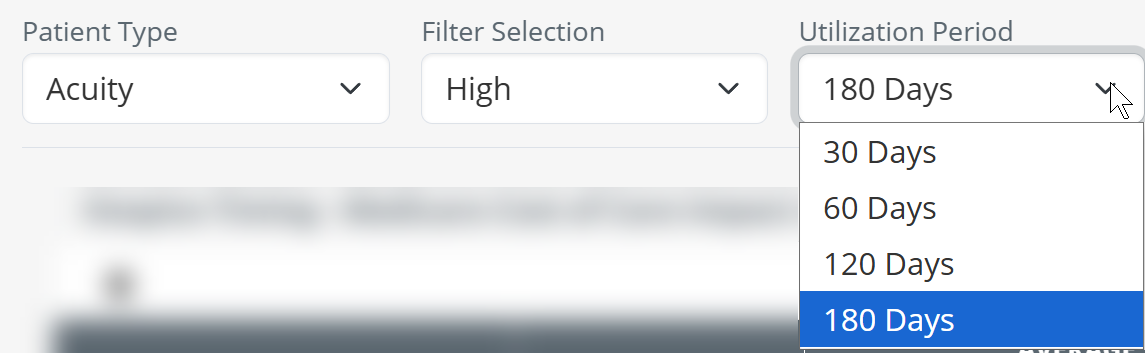 |
| Chronic Condition - the third patient type that you can choose is chronic condition. | 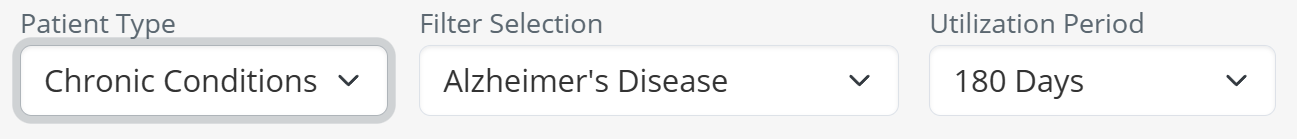 |
|
Choose a chronic condition - if you choose the Chronic Condition patient type, you then have the option to select a specific chronic condition from the second dropdown. The chronic conditions available are shown in the image to the right.
|
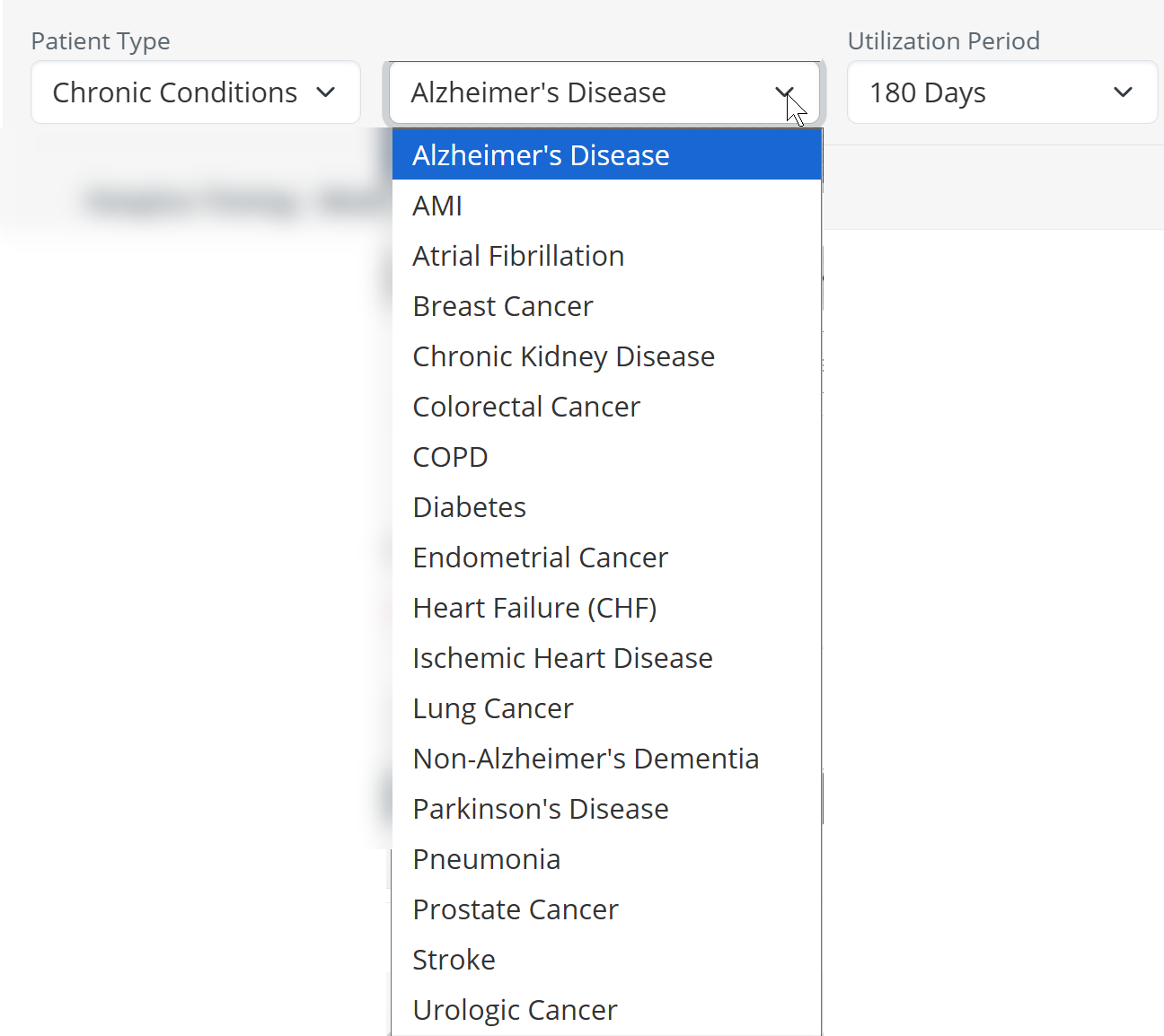 |
| Utilization Period - after you have chosen a specific chronic condition, you can choose to filter the results in the table to a specific period using the third dropdown. | 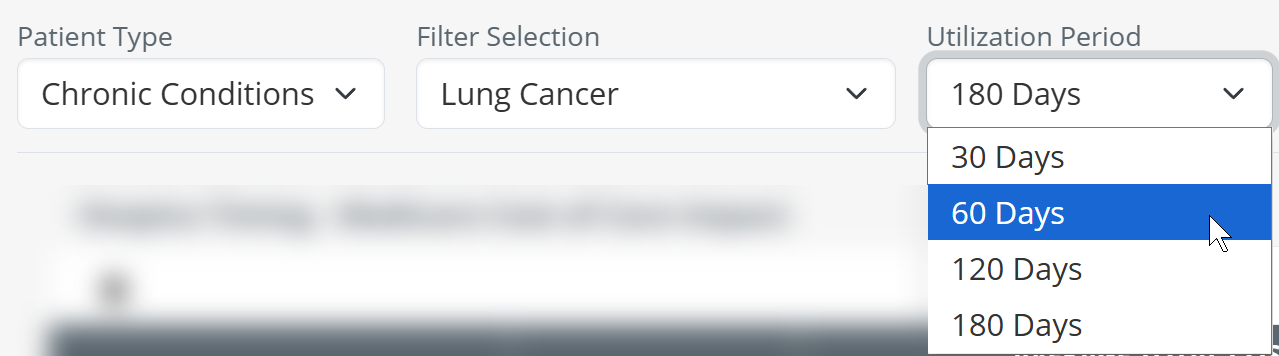 |
![]() Patients included in the counts for the different periods of hospice care could have potentially revoked hospice care, and also been re-admitted to hospice, or not. The variety of possible hospitalization scenarios are taken into consideration when we calculate the metrics in the table. In this table we only count hospice stays that are the last hospice admission prior to the patient's death.
Patients included in the counts for the different periods of hospice care could have potentially revoked hospice care, and also been re-admitted to hospice, or not. The variety of possible hospitalization scenarios are taken into consideration when we calculate the metrics in the table. In this table we only count hospice stays that are the last hospice admission prior to the patient's death.
Hospice Timing - Medicare Cost of Care Impact table and chart
The top table in the hospice timing panel focuses on the impact of earlier hospice care on costs.
Data Presentation
The metrics in the Medicare Cost of Care Impact table can be viewed as a table or as a chart.
![]() To enlarge an image, click on it.
To enlarge an image, click on it.
 Value
Value
The metrics in this table are designed to:
- Furnish insights into the financial and utilization impact of hospice timing on your own patient population
- Help hospice providers identify and enroll patients earlier, improving patient care while improving financial performance
- Provide benchmarking against state and national averages to guide clinical and operational strategies
But let's make this simple: Behold a convincing example.
![]() Observations
Observations
- The chart shows the cost improvements from hospice, instantly and obviously.
- Being admitted to any level of hospice saves money over no hospice care.
- Longer stays save costs over shorter stays.
- Hospice is good, use hospice.
And, yes, you can customize the chart to show the same kind of trend for patients with different acuity levels and different chronic conditions. Customize your proof to numerous specific situations.
 Calculation
Calculation
To determine which patients are included in costs, and to confirm which costs are counted, there are a few limits that are helpful to understand.
- Index event - since the Hospice Timing tables are designed to show the value of hospice, we start by identifying a patient's death. To be included in these metrics, the patient must have died. Patients who are still on hospice during the reporting period are not included in Hospice Timing metrics.
- Reporting period - the patient's death must have occurred during the one-year reporting period. This is the one-year period period ending on the last day of the most recently released data.
| The one year reporting period is identified at the top right of every page in Marketscape Insights. The relevant reporting period for this table is "Medicare Fee for Service (FFS)". The reporting period changes with each new release. |  |
- Discharge Reference period - from the patients who died during the reporting period, only patients who died within 180 days of discharge from the selected facility are included in the metric calculations.
-
No Hospice/Length of Stay - for patients that meet all of the above requirements, we break them up into the five categories shown in the chart and the table. The costs for these patients are displayed.
- No Hospice
- 0-14 Days on Hospice
- 15-60 Days on Hospice
- 61-120 Days on Hospice
- 121+ Days on Hospice
- Patient Type - You are able to use the dropdown filters to further limit the population from which the metrics are calculated into all patients, patients of a specific acuity level, and patients with specific chronic conditions.
- Lookback/Utilization period - Finally, you are able to choose a length of time from which the costs are calculated, 30 days, 60 days, 120 days, and 180 days. Use the image and examples below to see how costs are calculated.
Examples
Patient 1 was discharged 171 days before death and was on hospice care for the last 51 days.
- If we choose a 30 day period, only costs in the last 30 days would be counted. The costs would be used in the average for the column, 121+ days on Hospice, because the patient was on hospice 148 days.
- If we choose a 60 day period, costs that occurred in the last 60 days would be counted. The costs would be used in the average for the column, 121+ days on Hospice, because the patient was on hospice 148 days.
- If we choose a 120 day period, costs that occurred in the last 120 days would be counted. The costs would be used in the average for the column, 121+ days on Hospice, because the patient was on hospice 148 days.
- If we choose a 180 day period, costs that occurred in the last 180 days would be counted, even though some costs occurred prior to their hospice stay, and prior to their discharge. The costs would be used in the average for the column, 121+ days on Hospice, because the patient was on hospice 148 days.
Patient 2 was discharged 47 days before death and was on hospice care for the last 19 days.
- If we choose a 30 day period, only costs in the last 30 days would be counted, even though some costs occurred prior to hospice care. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 19 days.
- If we choose a 60 day period, costs that occurred in the last 60 days would be counted, even though some costs occurred prior to hospice care, and prior to their discharge. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 19 days.
- If we choose a 120 day period, costs that occurred in the last 120 days would be counted, even though some costs occurred prior to their hospice stay, and prior to their discharge. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 19 days.
- If we choose a 180 day period, costs that occurred in the last 180 days would be counted, even though some costs occurred prior to their hospice stay, and prior to their discharge. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 19 days.
Patient 3 was discharged 116 days before death and was on hospice care for the last 51 days.
- If we choose a 30 day period, only costs in the last 30 days would be counted. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 51 days.
- If we choose a 60 day period, costs that occurred in the last 60 days would be counted, even though some costs occurred prior to hospice care. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 51 days.
- If we choose a 120 day period, costs that occurred in the last 120 days would be counted, even though some costs occurred prior to their hospice stay, and prior to their discharge. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 51 days.
- If we choose a 180 day period, costs that occurred in the last 180 days would be counted, even though some costs occurred prior to their hospice stay, and prior to their discharge. The costs would be used in the average for the column, 15 - 60 days on Hospice, because the patient was on hospice 51 days.
![]() The image above has all three patients day of death the same in order to simplify the illustration. In real life, the dates of death could at any time in the one year reporting period and we would then look back from that date.
The image above has all three patients day of death the same in order to simplify the illustration. In real life, the dates of death could at any time in the one year reporting period and we would then look back from that date.
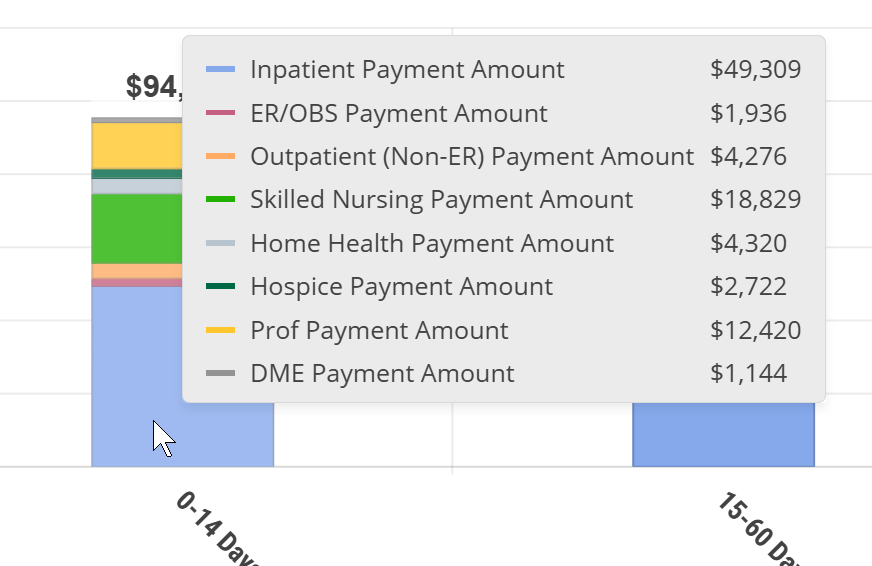
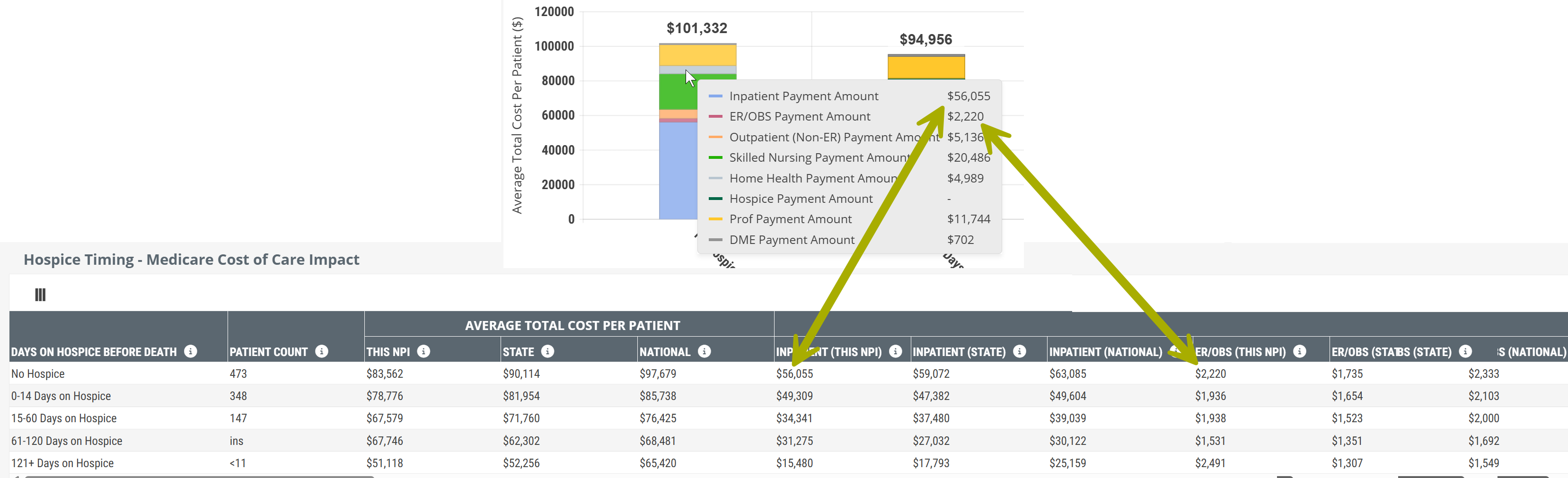
Chart versus Table
Since the content in the chart view and table view are the same, but presented differently, let's compare using the following image.
The image shows a small section of the table view with a section of the chart above including the metrics that are displayed when you hover over a bar in the chart. Specifically, we hovered over the "No Hospice" bar.
 Things to notice:
Things to notice:
- The chart makes it much easier to visualize trends.
- When you hover, you reveal specific metrics from the table. The arrows above show how the same metrics, related to your selected NPI, are included in the chart. The rest of the metrics shown in the hover are in the part of the table to the right that is not being shown.
- The table, in addition to other metrics, includes the state and national averages for comparison.
![]() We strongly suggest comparing the table to the chart. The chart is a powerful visual presentation that shows how earlier hospice impacts costs and utilization. The table provides a lot more detail for comparison and evaluation.
We strongly suggest comparing the table to the chart. The chart is a powerful visual presentation that shows how earlier hospice impacts costs and utilization. The table provides a lot more detail for comparison and evaluation.
Metric Details - Hospice Timing - Medicare Cost of Care Impact
The table includes ALL of the metrics included in the chart and more. The following list shows all metrics in the table which are also shown in the chart. Use the following image to compare to what you see on the Analyze page.
![]() We broke the table up into parts so that the whole table is presented in a way that is more readable. You can click on the above image to enlarge it, of see the complete table, here.
We broke the table up into parts so that the whole table is presented in a way that is more readable. You can click on the above image to enlarge it, of see the complete table, here.
Metric Name |
Description |
|
| Days on Hospice before Death | This column shows the reference time period from which the metrics in the same row are calculated. For example, the row "No Hospice" calculates metrics from claims of patients discharged from the selected facility who died without receiving any hospice care. The remaining rows contain metrics for patients who received the listed number of days under hospice care. | |
| Patient Count |
The count of distinct patients who died during the most recent 4 quarters who were discharged from the selected facility up to 6 months (180 Days) prior to death and who received the length of care listed in the row. |
|
|
| ||
|
Average Total Cost Per Patient |
Average total Medicare spend for patients discharged from the selected facility who received the length of care listed in the row.
|
|
|
Average Category Cost per patient
|
Inpatient | The average Medicare spend per patient on Inpatient claims (includes LTACH & IRF) for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. |
| ER/OBS | The average Medicare spend per patient on ER and observation claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
| Outpatient | The average Medicare spend per patient on outpatient claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
| SNF | The average Medicare spend per patient on skilled nursing claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
| Home Health | The average Medicare spend per patient on home health claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
| Hospice | The average Medicare spend per patient on hospice claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
| Professional | The average Medicare spend per patient on professional (Part B) claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
| DME | The average Medicare spend per patient on DME claims for patients discharged from the selected facility up to six months prior to death and who received the length of hospice care listed in the row. | |
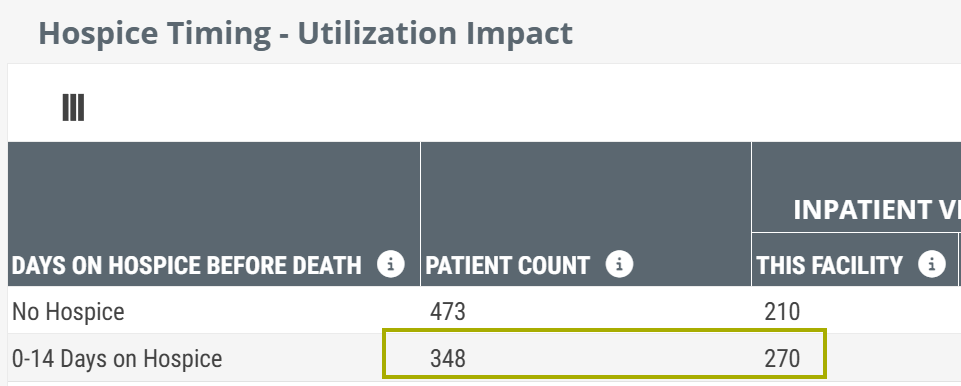
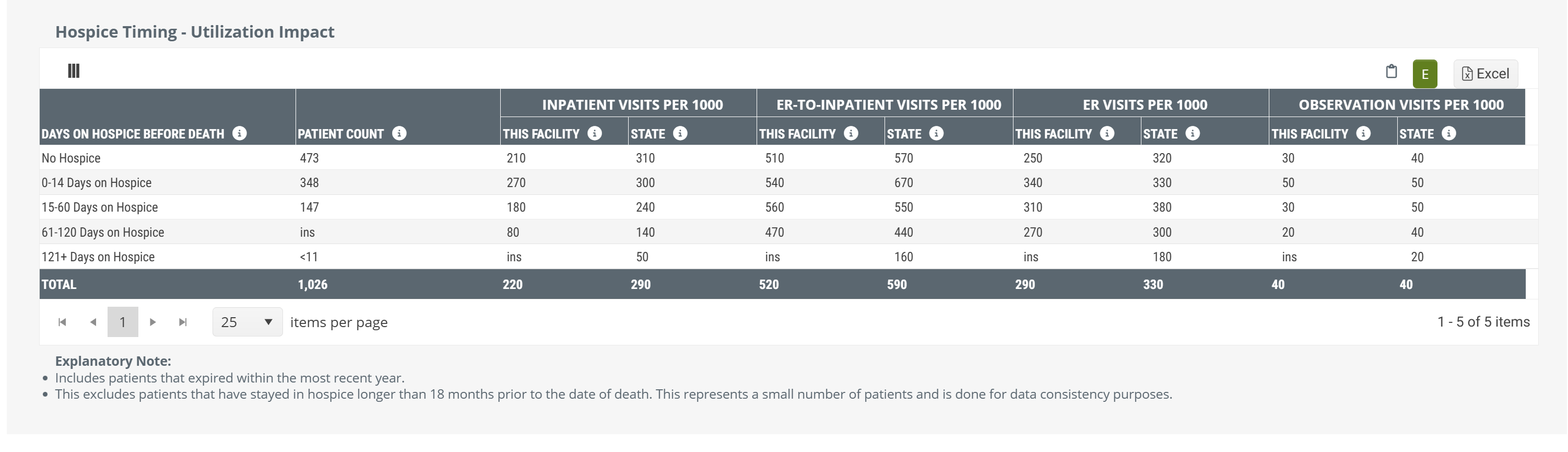
Hospice Timing - Utilization Impact table
For patients treated by a selected facility who died, we break that population into the following categories:
- No Hospice
- 0-14 Days on Hospice
- 15-60 Days on Hospice
- 61-120 Days on Hospice
- 121+ Days on Hospice
You can see these categories listed on the left side of the pictured table.
![]() Remember - the specific metrics shown in this table will depend on the filters you set.
Remember - the specific metrics shown in this table will depend on the filters you set.
Data Presentation
 Off Off
|
 |
 On On
|
There is no chart view for the metrics in this table. The table above is shown with Chart View on. |
![]() To enlarge an image, click on it.
To enlarge an image, click on it.
For each of these categories, this table provides overall patient counts for each category, and projected counts (per 1000 patients) for each of four different hospital levels of care.
 Value
Value
In light of the cost savings and benefits to patients and families that hospice care provides over hospitals for patients near the end of life, this table verifies the value of hospice care. For example, for each type of hospital visit, the table shows that early admission into hospice care is better than later admission, and that any hospice care is better than no hospice care at all.
This table makes it almost too easy to prove that getting hospice appropriate patients admitted to hospice care early is preferable. If you want to use these metrics in this way, most of the time you can prove this point using either the provider's metrics or the state averages.
Metric Name |
Description |
| Days on Hospice before Death | This column shows the reference time period from which the metrics in the same row are calculated. For example, the row "No Hospice" calculates metrics from claims of patients discharged from the selected facility who died without receiving any hospice care. The remaining rows contain metrics for patients who received the listed number of days under hospice care. |
| Patient Count | The count of distinct patients who died during the most recent 4 quarters who were discharged from the selected facility up to 6 months (180 Days) prior to death and who received the length of care listed in the row. |
| Inpatient | The average number of inpatient visits (not through the ER) per 1,000 patients who received the length of care listed in the row. |
| ER-to-Inpatient Visits per 1000 | The average number of inpatient visits (admitted through the ER) per 1,000 patients who received the length of care listed in the row. |
| ER Visits per 1000 | The average number of ER visits discharged home (not admitted to inpatient or observation) per 1,000 patients who received the length of care listed in the row. |
| Observation Visits per 100 | The average number of observation visits per 1,000 patients who received the length of care listed in the row. |
Usage
![]() Although the image shows metrics from a hospital Analyze page, the Hospice Timing table for a physician would provide the same use case.
Although the image shows metrics from a hospital Analyze page, the Hospice Timing table for a physician would provide the same use case.
 The value of hospice
The value of hospice
In light of the cost savings and benefits to patients and families that hospice care provides over hospitals for patients near the end of life, this table verifies the value of hospice care. For each type of hospital visit, the table shows that early admission into hospice care is better than later admission, and that any hospice care is better than no hospice care at all. We will look at the numbers below.
![]() This table makes it almost too easy to prove that getting hospice appropriate patients admitted to hospice care early is preferable. If you want to use these metrics in this way, most of the time you can prove this point using either the provider's metrics or the state averages.
This table makes it almost too easy to prove that getting hospice appropriate patients admitted to hospice care early is preferable. If you want to use these metrics in this way, most of the time you can prove this point using either the provider's metrics or the state averages.
 State metrics for comparison
State metrics for comparison
In addition to metrics specific to the selected provider, the table provides state averages for similar providers. The comparative nature of these metrics allows you to see how your selected provider performs against peers. If your selected provider underperforms or overperforms against peers, you will want to do some careful evaluation of the demographics of the patient population to find out why.
![]() You will want to be careful relaying these metrics to a physician. Although for a high performer you could communicate, "Hey, you're doing great!" it is important to dig in on why the physician's metrics are so good. If the metrics show poor performance against the state averages, you would want to only provide these insights in a context of trust and with a persuasive message of how you can help.
You will want to be careful relaying these metrics to a physician. Although for a high performer you could communicate, "Hey, you're doing great!" it is important to dig in on why the physician's metrics are so good. If the metrics show poor performance against the state averages, you would want to only provide these insights in a context of trust and with a persuasive message of how you can help.
![]() Keep in mind that these metrics also reflect on the care provided by all hospices that treated the provider's patients. This means that, for this table, the metrics do not provide insights into the success of your agency.
Keep in mind that these metrics also reflect on the care provided by all hospices that treated the provider's patients. This means that, for this table, the metrics do not provide insights into the success of your agency.
 Patient mix between categories
Patient mix between categories
The patient counts are a breakdown of the selected provider's patients who died during the reporting period.
![]() The sample image of a provider's metrics (above) demonstrates the need. This patients break down thus:
The sample image of a provider's metrics (above) demonstrates the need. This patients break down thus:
|
|
Considering the value of hospice care, these numbers are upside down. The message is clear. This provider needs help to identify hospice appropriate patients and get them admitted to hospice earlier.
 Hospital events
Hospital events
There are four hospital events that we track for hospice patients in this table.
- Inpatient Visits per 1000 - A patient is admitted to a hospital for inpatient care.
- ER-to-Inpatient Visits per 1000 - a patient is admitted to inpatient care through the emergency room.
- ER Visits per 1000 - a patient is taken to the emergency room, but not admitted for other additional care.
- Observation Visits per 1000 - a patient stays overnight for observation but is not admitted to inpatient care.
![]() The metrics in this table are based on visit counts, not patient counts. That is, a single patient could be counted multiple times for any level of hospital care, and counted for more than one type of hospital care.
The metrics in this table are based on visit counts, not patient counts. That is, a single patient could be counted multiple times for any level of hospital care, and counted for more than one type of hospital care.
Why do we use "Visits per 1000?"
The metrics in this table are the easiest to use and yet, it is challenging to understand the math. As a result, when someone asks, "Why use Visits per 1000," the answer is that we want to make it easy to compare the bottom line insights provided by the table without being forced to work through complicated metrics.
But, if you feel compelled to press further about the use of "Visits per 1000, we provide a simple answer and a real mathy answer.
Simple Answer
Trust Trella Health.
Our data scientists spend a lot of time to assure that our metrics are accurate and useful. So it is wise to focus on the purpose of this table. This table shows the value of getting patients into hospice care as early as possible.
If you look at the image below - Inpatient Visits per 1000 for the selected facility (This Facility). We see some numbers; 210, 270, 180, and 80.
Forget about the "per 1000" for a second, and let's do a comparison thinking only about caring for patients.
- If we look at patients who had no hospice, or only a very short stay (0 - 14 days) that represents 480 patients. (per thousand.)
- That is six times as many inpatient admissions than patients who were under care between 61 - 120 days.
- If those 480 patients had been under care for 61 - 120 days, four hundred of them would not have been admitted to inpatient care.
![]() Bottom line - Early Hospice is better for the patients, and the numbers prove it! The cost savings and the improvement to end of life experience is enormous.
Bottom line - Early Hospice is better for the patients, and the numbers prove it! The cost savings and the improvement to end of life experience is enormous.
![]() Keep in mind that the "per 1000" counts don't represent actual patients, they are numbers that we calculate in order to provide a comparison of the different hospice timing scenarios for the selected hospital or physician. Read on if you want to understand why and how we do this.
Keep in mind that the "per 1000" counts don't represent actual patients, they are numbers that we calculate in order to provide a comparison of the different hospice timing scenarios for the selected hospital or physician. Read on if you want to understand why and how we do this.
 Lotsa Math
Lotsa Math
Now let's jump into why we do this.
Imagine that we wanted to figure out the average number of times a group of people go to the grocery store each month. We will start with a small group.
From the image we see the number of trips each person in our group took. We add the trips together and then divide by the number of people in the group.
3 + 2 + 4 + 5 = 14 total trips for groceries in the month
14 / 4 = 3.5 trips - the average number of trips for our group.
If we do the same for a bigger group, the process is the same
3+3+3+2+5+2+4+2+5+3+3+4+4+3+2+4+2+2+3+5+3+5+3+4 = 79
79 / 24 = 3.3 trips/month (rounded from 3.2916667)
Some observations:
- No matter how many people are in our group, the process is the same.
- If one or two or even a few of our shoppers never went to the grocery store, we would still get an average that makes sense.
But consider what happens when we change what we are looking for.
For the same 24 people from the last calculation, let's get an average number of times those same people gave blood at Red Cross in the same month:
Only three people gave blood, so the average is:
3 / 24 or .125 donations per month, or, the average number of donations in a month is 1/8 (one eighth) of a donation. Although the math works, conceptually that is a hard way to think about averages.
![]() Historical Note: For the first pass of this table we included the averages, but often the metrics were so small that most users had difficulty making sense of them. For example, what is an average of .02 visits?
Historical Note: For the first pass of this table we included the averages, but often the metrics were so small that most users had difficulty making sense of them. For example, what is an average of .02 visits?
The Solution
An easier way to show the comparative value of this metric is to display an "out of 1000" count.
So, looking at our table again, we can see that for the 348 patients represented who had 0-14 days of hospice, we have an inpatient admission count of 270 visits per 1000 patients.
 What does this mean?
What does this mean?
The way to read this is, based on the patient count and the number of visits (admitted to inpatient care), IF we had 1000 patients in our no hospice group, we expect that 270 of them would be admitted to inpatient care.
 Finally, some Calculations
Finally, some Calculations
The final mystery is, how many actual visits are we talking about. Oddly, we can figure this out.
The "Visits per 1000" count is 270. So we divide 270 by 1000
270 / 1000 = .27
Multiply .27 times 348 - the number of patients from the group of those who would have been admitted to inpatient care. The answer is 93.96, which we round to 94.
Obviously, to calculate the 270 per 1000, we went the other way.
The calculation is:
Here are the steps we followed.
- Get a count of deceased patients who were not admitted to hospice - 348
- Count how many of those patients were admitted to inpatient care - 94 (a number we don't we don't show in the table.)
- Divide the 94 visits by 348 patients
 94 visits per (divide) 348 patients = .2701149 visits per patient.
94 visits per (divide) 348 patients = .2701149 visits per patient. - Multiply by 1000
 .2701149 X 1000 = 270.11
.2701149 X 1000 = 270.11 - Round to the nearest whole number
 270
270
And that is the number we see in the column for visits per 1000 patients.
This is one of those times where we say, "these are trained mathematicians, don't try this at home."
The reason is that when you work this kind of math backward and forward, the rounding of numbers invariably will leave you a number that doesn't match when you work backwards.